Choose the content to read
- What is blood in stool or rectal bleeding?
- Why the color of the stool matters?
- What are the causes of rectal bleeding or blood in stool?
- What causes blood in stool in children?
- How is the cause of blood in stool diagnosed?
- How is blood in stool or rectal bleeding treated?
- FAQ
Blood in Stool (Rectal Bleeding)
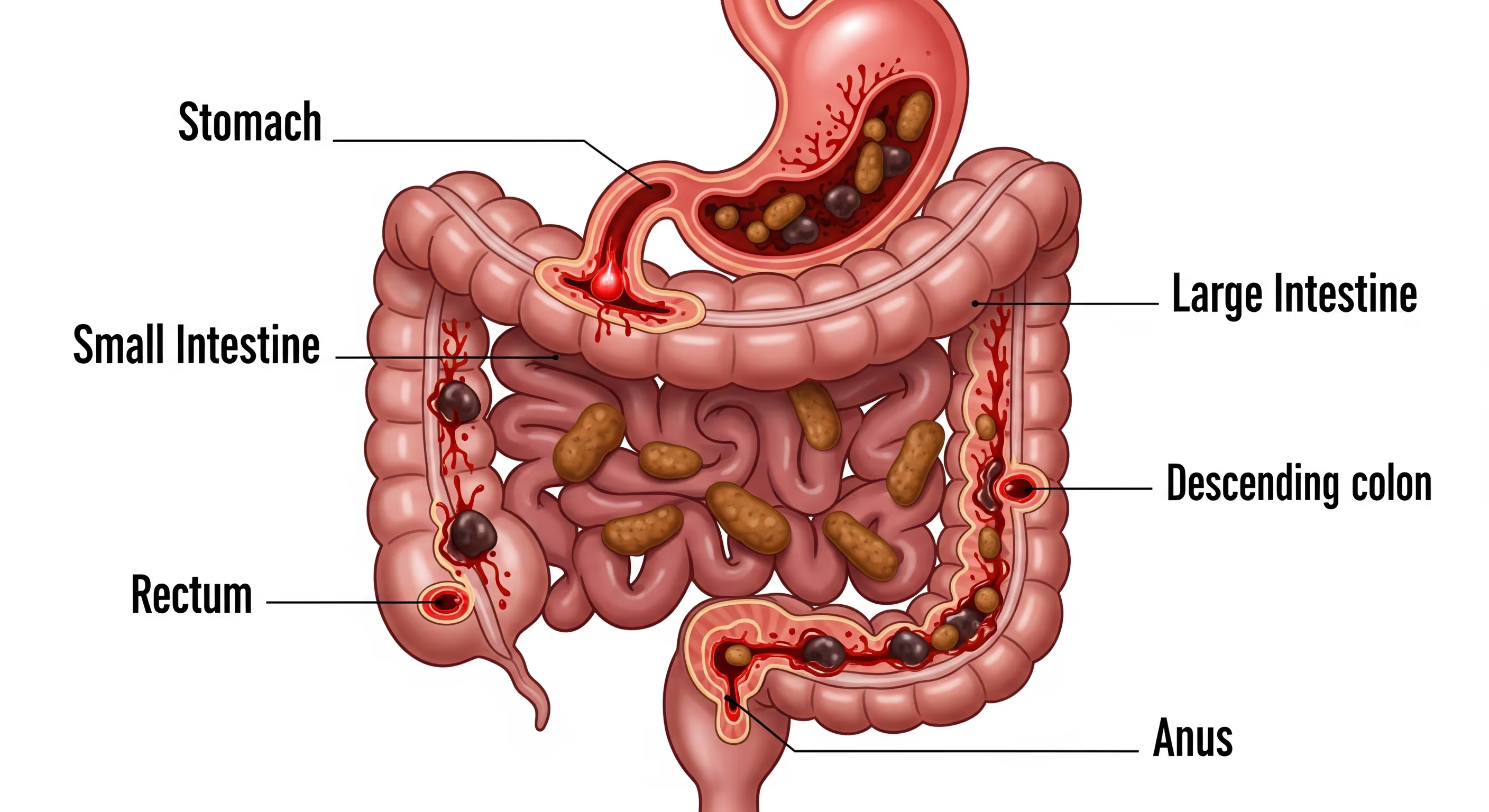
Blood in stool is a manifestation of gastrointestinal bleeding that can result from a variety of underlying conditions, including hemorrhoids, anal fissures, and chronic inflammatory bowel diseases, or more serious pathologies such as gastric and colorectal cancers. When blood in stool occurs or if stool appears bright red or black, it is advisable to seek prompt medical attention for accurate diagnosis and appropriate management.
What is blood in stool or rectal bleeding?
Blood in stool or Rectal Bleeding, also known as hematochezia, refers to the passage of blood with stool. The source of the bleeding may originate from either the upper or lower gastrointestinal tract, including the stomach, small intestine, colon, rectum, and anus. While often it is due to minor issues like hemorrhoids or anal fissures, it can also be a sign of more serious conditions, such as peptic ulcers, inflammatory bowel disease, intestinal tuberculosis, or colorectal cancer.
Why the color of the stool matters?
The color of the blood can provide important clues about the site of the bleeding.
- Bright red blood passed with stool often suggests bleeding from a lesion near the anus, such as an anal fissure or hemorrhoids.
- Dark red, maroon, or reddish-black stool indicates bleeding from a more proximal part of the gastrointestinal tract, such as the colon or small intestine.
- In some cases, the stool may appear black, tarry, and foul-smelling (a condition known as melena), which suggests bleeding from the upper gastrointestinal tract, such as the stomach or duodenum.
In some patients, only a minute amount of blood is present in the stool—too small to be detected with the naked eye—yet it can be identified through laboratory testing using the Fecal Occult Blood Test (FOBT). This diagnostic method is capable of detecting minimal gastrointestinal bleeding and is a commonly used screening tool for colorectal cancer.

When to see a doctor?
You should seek medical evaluation regardless of the amount of blood present in the stool. If uncertain, doctors can send stool for laboratory analysis using the aforementioned Fecal Occult Blood Test (FOBT). Even a trace amount of blood detected through this test may indicate an underlying intestinal disorder, requiring treatment that you should not ignore. Conversely, if a significant amount of blood is visible to the naked eye or if the stool appears black, this suggests substantial gastrointestinal bleeding. In particular, the presence of accompanying symptoms such as dizziness warrants immediate medical evaluation.
What are the causes of rectal bleeding or blood in stool?
- Hemorrhoids often develop due to excessive straining during bowel movements or habitual prolonged toilet sitting, particularly in individuals with chronic constipation. Common symptoms include itching or pain around the anus.
- Anal fissures are small tears in the lining of the anus, often caused by the passage of hard or bulky stools, leading to sharp pain and bright red bleeding.
- Inflammatory bowel disease (IBD), including ulcerative colitis and Crohn’s disease, though relatively uncommon in Thailand, causes chronic inflammation of the gastrointestinal tract. Symptoms may include bloody diarrhea, abdominal pain, fatigue, and unintentional weight loss.
- Ischemic colitis occurs when blood flow to the colon is insufficient, leading to tissue ischemia and necrosis, which may result in abdominal pain, tenderness, and bloody diarrhea.
- Diverticular disease may cause gastrointestinal bleeding, abdominal pain, or the passage of blood in the stool if a pouch becomes inflamed due to infection, or rupture of blood vessel at the neck of a diverticulum, it may result in gastrointestinal bleeding, abdominal pain, or the passage of blood in the stool.
- Sexually transmitted infections (STIs) such as gonorrhea, chlamydia, herpes simplex, and syphilis can cause inflammation of the rectal mucosa, leading to bleeding. In addition, anal intercourse may cause irritation or trauma, resulting in rectal bleeding.
- Colitis may result from infection of the large intestine or inflammation caused by autoimmune disorders. It typically presents with fever, abdominal pain, and stools containing bloody mucus.
- Angiodysplasia refers to abnormal or ectopic blood vessels that develop in the intestinal lining. These fragile vessels can rupture easily upon contact with stool, leading to bleeding.
- Peptic ulcers are most commonly due to infection with Helicobacter pylori or the long-term use of nonsteroidal anti-inflammatory drugs (NSAIDs), including aspirin or ibuprofen.
- Colorectal polyps or colorectal cancer can cause intestinal bleeding that is often not visible to the naked eye and may only be detectable through colorectal cancer screening.
- Esophageal varices or Mallory–Weiss syndrome can lead to significant upper gastrointestinal bleeding, often presenting as hematemesis or melena.
- Anticoagulant medications, such as aspirin or warfarin, may increase the risk of gastrointestinal bleeding, sometimes resulting in black stools.
- Bacterial gastroenteritis caused by Escherichia coli, Salmonella, Shigella, or Campylobacter can result in diarrhea mixed with blood, nausea, vomiting, and abdominal cramps.
- Endometriosis may involve areas near the anus or within the rectal wall, leading to rectal bleeding during menstruation.
- Gastrointestinal bleeding can occur anywhere from the esophagus and stomach to the colon, rectum, and anus, leading to vomiting of blood, passage of black, tarry stools, or fresh blood in the stool. Associated symptoms can include fatigue, dizziness, chest tightness, or shortness of breath.

What causes blood in stool in children?
- Constipation is the leading cause of rectal bleeding.
- Peptic ulcers are most commonly attributed to infection with Helicobacter pylori, and may present with symptoms such as melena (black, tarry stools), epigastric pain, or frequent belching.
- Food allergies, particularly to cow’s milk protein, eggs, peanuts, wheat, fish, or seafood—sometimes present in formula or transmitted via breast milk—can lead to intestinal inflammation and bleeding.
- Infectious diarrhea can result from ingesting food or water contaminated with a virus, bacteria, or parasites.
- Meckel’s diverticulum is a congenital outpouching in the distal small intestine that may contain acid-secreting gastric tissue, leading to gastrointestinal bleeding. This condition is most commonly observed in young children and can be treated surgically by removing the diverticulum.
- Inflammatory bowel disease (IBD) includes Crohn’s disease and ulcerative colitis.

How is the cause of blood in stool diagnosed?
- Nasogastric lavage involves inserting a tube through a nostril into the stomach to aspirate gastric contents for the evaluation of possible gastrointestinal bleeding.
- Esophagogastroduodenoscopy (EGD) is a procedure in which a small, flexible endoscope is passed through the mouth into the esophagus, stomach, and proximal duodenum to identify the source of bleeding. During the procedure, doctors can obtain tissue biopsies if necessary.
- Colonoscopy is an endoscopic procedure in which a flexible scope is inserted through the anus to examine the interior of the colon. It enables the identification of bleeding sites, inflammation, or polyps, and tissue samples can be obtained for laboratory analysis if needed.
- Enteroscopy involves the ingestion of a small capsule equipped with a camera, which captures images of the small intestine—areas that are not reachable by conventional endoscopy.
- Barium X-ray involves the patient ingesting or receiving a barium enema, which enhances the visibility of the gastrointestinal tract on X-ray imaging.
- In radionuclide scanning, clinicians inject a small amount of radioactive tracer intravenously and use a specialized camera to track its movement, allowing them to localize the site of bleeding.
- Angiography is a diagnostic procedure in which radiologists inject a contrast agent into the blood vessels and take a series of X-ray images. If bleeding is present, the contrast may leak from the bleeding vessel, enabling doctors to identify the exact site of hemorrhage.
- Anoscopy is an examination of the anus to detect abnormalities such as anal fissures, hemorrhoids, or localized bleeding.
- Proctoscopy involves the insertion of a scope into the rectum and anus to evaluate for abnormalities or lesions in the rectum.
- Flexible sigmoidoscopy is an endoscopic examination of the distal colon, providing sharper images than proctoscopy. It can detect inflammation, bleeding, or other abnormalities.
- A rectal culture swab can identify bacterial pathogens that may cause bleeding or inflammation.
- Stool testing is a laboratory analysis of stool samples to detect occult blood, infections such as H. pylori, causes of anemia, or coagulation disorders.
- A computed tomography (CT) scan can identify inflammation, tumors, and other conditions.
- Laparotomy is an open abdominal surgical procedure to examine the internal organs. Doctors resort to this procedure when other diagnostic methods fail to determine the cause of gastrointestinal bleeding.

How is blood in stool or rectal bleeding treated?
Rectal bleeding caused by constipation often resolves without the need for specific treatment. In mild cases, doctors may recommend a high-fiber diet to alleviate constipation and alleviate straining during bowel movements, along with regular physical activity to promote normal bowel function. If symptoms are severe or arise from other causes, treatment may include:
- Medications: such as antibiotics to treat H. pylori infection, acid-suppressing agents for gastric ulcers, or anti-inflammatory drugs for patients with inflammatory bowel disease.
- Surgery: to remove polyps, cancerous or damaged segments of the intestine, inflamed diverticula, or bowel segments affected by chronic inflammatory bowel disease.
- Endoscopic hemostasis: using techniques such as injection therapy, thermal coagulation, laser therapy, or banding/clipping of bleeding vessels during endoscopy.
- Angiographic intervention: to deliver medication at the site of bleeding, helping to control hemorrhage. This approach is typically employed when other methods have been unsuccessful.
Summary of blood in the stool symptoms
Rectal bleeding or Blood in stool is a symptom that indicates a pathological condition within the gastrointestinal tract. Its causes can range from non-severe conditions, such as hemorrhoids, to serious diseases like colorectal cancer. The appearance of the blood can help in the preliminary assessment of the bleeding's location; bright red blood often indicates an abnormality in the lower large intestine, while darker blood may originate from a higher position in the digestive tract. Therefore, in any case of rectal bleeding, patients should seek a prompt medical diagnosis to identify the cause and plan for appropriate treatment. Treatment approaches range from medication and endoscopic procedures to surgery.
Preparing for your doctor’s visit
Before your appointment, keep a record of your symptoms and prepare a list of questions:
- Is my condition serious?
- What diagnostic tests and treatment options do you recommend?
- What steps can I take to relieve my symptoms or prevent rectal bleeding from recurring?
Frequently Asked Questions (FAQ)
- Should I be worried if I notice blood in my stool?
If blood is present in the stool, careful monitoring of symptoms is essential, particularly when the underlying cause is unknown. Blood in the stool may serve as a warning sign of gastrointestinal disease. Significant, frequent, or persistent bleeding lasting more than one week can lead to anemia and, in severe cases, may result in shock. Prompt medical evaluation and appropriate treatment are therefore strongly recommended. - Is blood in the stool always a serious issue?
Bleeding may result from mild conditions such as constipation or anal fissures, which often resolve on their own. Nonetheless, it is crucial to consult a doctor to determine the underlying cause and assess whether medical treatment is necessary. - Is bright red blood more concerning than dark-colored blood?
Bright red blood in the stool usually originates from the anus or rectum. A black or dark tarry stool may indicate bleeding in the upper gastrointestinal tract, such as the stomach or small intestine, where enzymatic digestion of blood darkens its color. Regardless of whether the blood appears bright red or dark, medical evaluation is strongly advisable. - Can straining during bowel movements cause rectal bleeding?
Excessive straining during bowel movements can lead to hemorrhoids or anal fissures, which are common causes of rectal bleeding. - Are the causes of rectal bleeding in children the same as in adults?
Children who pass blood in their stool most commonly have anal fissures caused by constipation or infectious colitis. In contrast, chronic conditions such as inflammatory bowel disease, diverticular disease, or colorectal cancer are more frequent in adults. - Are the causes of rectal bleeding different between men and women?
The causes are generally similar in both sexes. However, some women may experience increased anal irritation or rectal bleeding during menstruation due to hormonal changes or elevated pelvic pressure. - Can certain foods cause red-colored stool?
Stool may appear red after consuming certain foods, such as beets, blackberries, tomatoes, or foods containing red food coloring. Additionally, iron supplements and certain medications can cause the stool to appear black.
A Note from MedPark’s Doctors
Blood in Sool or Rectal bleeding can be caused by a variety of conditions, from minor issues that are easily treatable to serious illnesses that require urgent medical attention. Seeking prompt medical care is the crucial first step to an accurate diagnosis and the correct treatment, which increases the chances of a successful outcome and helps prevent complications.

















