Kidney Transplant: Rekindling Health and Hope in End-Stage Renal Disease
The term end-stage renal disease can evoke fear, despair, and desperation. At this advanced stage, treatment options are limited, and nearly all available interventions entail significant compromises to quality of life. Yet one approach offers the most effective outcomes, restoring patients’ quality of life to the greatest extent possible, though it is also the most challenging procedure: kidney transplantation.

End-Stage Renal Disease and the Kidney Transplantation
Dr. Teerayuth Jiamjariyapon, a transplant nephrologist, explains that kidney transplantation is a treatment option for patients with stage 5 chronic kidney disease or end-stage renal disease. Patients at this stage generally have three treatment options: hemodialysis, peritoneal dialysis, and kidney transplantation. Among these, kidney transplantation is the most complex and challenging procedure, but it also offers the most effective outcomes.
“Clinical studies have shown that kidney transplantation can sustain the life of patients with kidney disease more effectively than other treatments and quickly restore their quality of life.”
In discussing kidney transplantation, Dr. Teerayuth noted that the procedure can proceed if the patient does not have the following contraindications:
- Untreated heart disease or cancers
- Active infections, such as severe hepatitis
- Other significant health-related restrictions
The key advantage of this treatment is that it requires just one-time surgery, eliminating the need for dialysis sessions every 2 days or several times a week. Patients typically see noticeable improvements soon after.

The Challenges of Kidney Transplantation in Thailand
“The biggest challenge is finding a suitable donor kidney for the patient,” Dr. Teerayuth said without hesitation when asked about the obstacles in kidney transplantation.
Donated kidneys generally come from two sources:
- Living donors, typically family members, are the most optimal option.
- Cadaveric donors, or kidneys procured through the central bureau (Thai Red Cross), require patients to register for placement on the waiting list for brain-dead donors. This process often involves a lengthy waiting period.
In addition, kidney transplantation requires an orchestrated collaboration among a highly skilled and experienced multidisciplinary team, including transplant nephrologists and urologic surgeons. When necessary, the team also consults with other specialists to manage patients with comorbidities, such as cardiovascular disease, cerebrovascular disorders, gastrointestinal conditions, and more.
“For patients over the age of 50, a colonoscopy should be performed to screen for colorectal cancer. An infectious disease specialist should also assess whether any latent viral infections are present, and give necessary vaccinations to prevent potential future infections.”
Another crucial member of the kidney transplant care team is a psychiatrist who assesses mental health, particularly when the stress and anxiety caused by illness affect the patient and their family members.
Matching Organ Donors with Recipients: A Pivotal Task for Nephrologists
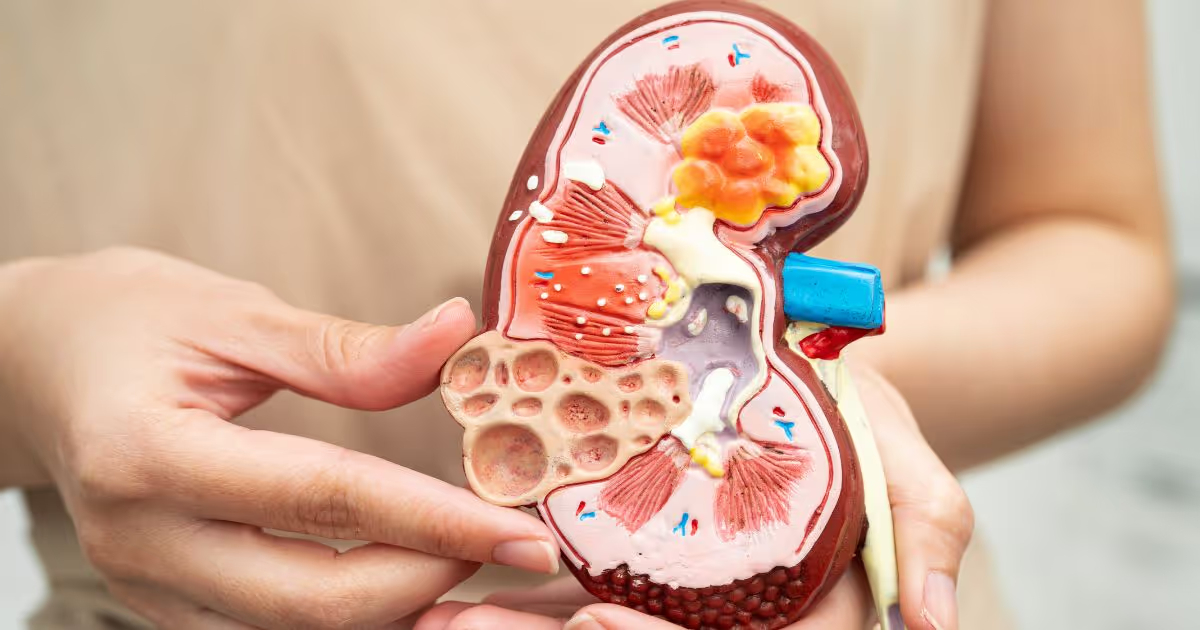
Dr. Teerayuth explains that compatibility matching of a kidney donor and a recipient is crucial to ensure the long-term function and lifespan of the transplanted kidney. This process involves complex procedures and meticulous protocols."
“To assess compatibility, we mix the blood of the kidney donor and the recipient in vitro. Nowadays, performing immunological testing yields more detailed results, enabling accurate identification of compatible matches. When transplanting a well-matched kidney, it can function physiologically for many years.”
“A new technology called plasma exchange allows kidney transplantation in patients with pre-existing antibodies. This procedure requires the expertise of medical technologists while the transplant nephrologist reviews the laboratory test results and determines whether the donated kidney is safe for transplantation into the patient.”
As to the longevity of a transplanted kidney, it typically lasts from 10 to 20 years, depending on the patient’s health and the degree of compatibility between the donor kidney and the recipient.
Legal Considerations for Kidney Donation and Transplantation Everyone Should Know
Under Thai law, living kidney donations must come from blood relatives or direct descendants, such as a child donating to a parent or a grandchild donating to an uncle. The transplant team carefully reviews all supporting documents. For spousal donations, the couple must have been legally married and registered for at least three years.
For deceased donors, the Thai Red Cross clearing house allocates kidneys from brain-dead individuals based on the waiting list and the compatibility between the kidney donor and the recipient.
Transplantation of kidneys outside the legally sanctioned framework is strictly forbidden. In the case of living donors, only those who fulfill the established legal and medical requirements are eligible to donate.
MedPark Hospital’s Commitment to Treating Kidney Disease Patients Through Kidney Transplantation
MedPark Hospital has a dedicated team of doctors and healthcare professionals skilled in performing kidney transplant surgeries. To date, the hospital has successfully conducted living kidney transplants in five patients, meeting the criteria for consideration as a member of the Thai Red Cross to receive organs from the central allocation system.
“At present, MedPark holds the status of an associate member. We have completed the required number of living-donor transplants, typically from relatives. Looking ahead, we anticipate that once the Thai Red Cross elevates our status to an ordinary member, the hospital will be able to receive donated kidneys for transplantation and provide care to a larger number of patients.”

Dr. Teerayuth emphasizes that fostering understanding and trust in the kidney donation among family members is essential for enhancing future kidney disease treatment options. This potential source is the most effective and convenient, offering the highest likelihood of compatibility between the donor kidney and the recipient. Moreover, modern surgical techniques have advanced by leaps and bounds, utilizing robotic-assisted surgery, which minimizes the risk of complications.
“A key factor is increasing the number of donors. In countries such as Spain, for example, if a person killed in a car accident is declared brain-dead, the government legally authorizes the retrieval of organs for transplantation. Consent for organ donation is often given at the time of obtaining a driver’s license, making the process rightfully lawful. In Thailand, efforts are increasingly being made to raise awareness and understanding about body and organ donation. A single donor can save the lives of multiple patients, and donors may be honored with a royal cremation, which serves to encourage donation and alleviate cultural concerns or fears that the body may not be whole in the next life.”
Dr. Teerayuth also noted that genetically modified pigs could be a source of kidneys for xenotransplantation as an alternative to human organs. This approach has seen short-term success in at least three cases in the United States. It represents a promising avenue for treating patients with end-stage kidney disease, particularly considering the growing demand for donor kidneys and the persistent shortage of available organs. Currently, this method remains in the early experimental phase of research.

Prevention: The Best Strategy Against End-Stage Chronic Kidney Disease
“The insidious nature of kidney disease lies in the absence of early symptoms. By the time abnormalities appear, the disease has inevitably progressed to an advanced stage. Early screening and lifestyle modifications to prevent the onset of kidney disease are therefore the most effective strategies for managing this condition.”
For individuals who are currently healthy and wish to prevent kidney disease, maintaining overall health is essential. Dr. Teerayuth recommends the following measures:
- Keep systolic blood pressure below 130 mmHg
- Monitor blood sugar levels, particularly for patients with diabetes
- Undergo regular annual health check-ups
By being vigilant and prioritizing overall health, it is possible to prevent chronic diseases that compromise quality of life, leading to frequent hospital visits, substantial time loss, and financial burdens.












