大便带血(直肠出血)
大便带血是消化道出血的一种表现形式,可能由多种基础疾病引起,包括痔疮、肛裂、慢性炎症性肠病等,也可能与较为严重的疾病有关,如胃癌或结直肠癌。当出现大便带血,或大便呈鲜红色、暗红色甚至黑色时,建议尽早就医,以便进行准确诊断和及时治疗。
什么是大便带血或直肠出血?
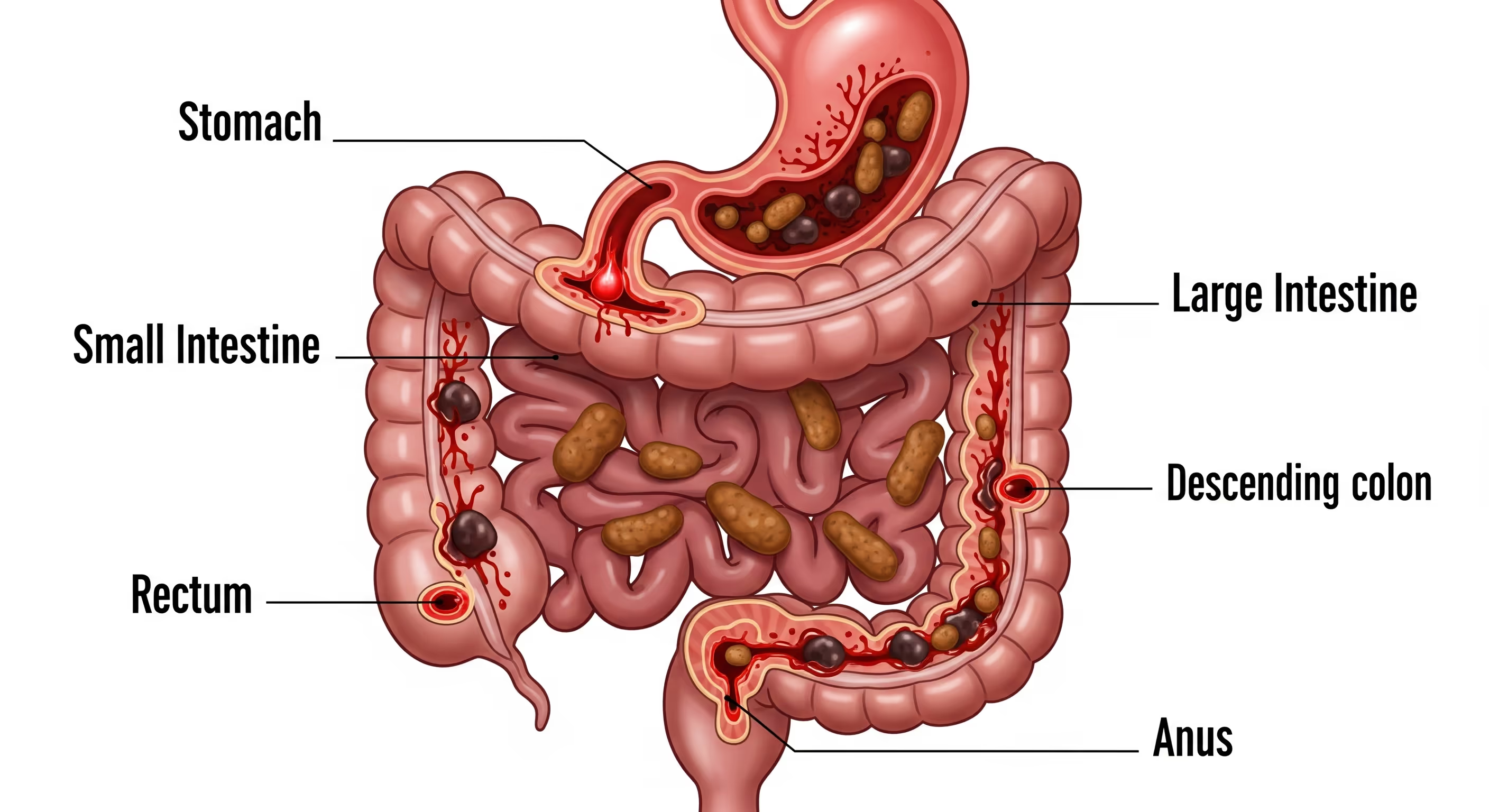
大便带血或直肠出血(医学上称为“血便”或“下消化道出血”,hematochezia),是指排便时粪便中混有血液。出血来源可来自上消化道或下消化道,包括食管、胃、小肠、结肠、直肠及肛门。虽然多数情况下与痔疮或肛裂等良性疾病有关,但也可能提示更严重的问题,如消化性溃疡、炎症性肠病、肠结核或结直肠癌。
何时需要就医?
无论出血量多少,只要发现大便中带血,都应接受医生评估。如无法确定是否存在出血,医生可安排粪便隐血试验(FOBT)进行检测。即使仅检测到微量隐血,也可能提示肠道疾病,需进一步检查和治疗,不应忽视。
若肉眼可见大量鲜血,或大便呈黑色(柏油样便),通常提示较严重的消化道出血。如伴随头晕、乏力等症状,应立即就医。
为什么大便颜色值得关注?
大便颜色的变化,尤其是伴随血液出现时,往往为胃肠道出血的部位提供重要线索。及时识别这些信号,有助于早期发现潜在疾病并进行有效治疗。
- 鲜红色血液:多提示出血来源于肛门附近的病变,如肛裂或痔疮。
- 暗红色、棕红色或黑红色大便:通常提示出血来自较靠近上端的胃肠道部位,如结肠或小肠。
- 黑色、柏油样且伴有恶臭的大便(黑便):提示出血可能来自上消化道,如胃或十二指肠。
部分患者大便中可能仅含有极少量血液,肉眼无法察觉。此时可通过实验室检查——大便潜血试验(FOBT)进行检测。该方法能够发现微量胃肠道出血,是结直肠癌常用的筛查工具。

为什么需要及时就医?
无论粪便中血量多少,都应进行医学评估。若情况不明确,医生可通过实验室检查,如粪便潜血试验(FOBT),来检测是否存在血液。即使仅发现微量血液,也可能提示潜在的肠道疾病,需要及时治疗,不可忽视。
相反,如果肉眼可见大量血液,或粪便呈黑色,则提示胃肠道存在明显出血。尤其是伴随头晕等症状时,更需立即接受医学评估。
大便带血或直肠出血的常见原因
- 痔疮:多因排便用力过度、长期便秘或久坐如厕引起,常伴有肛门瘙痒或疼痛。
- 肛裂:肛管黏膜出现小裂口,多由干硬或粗大的粪便造成,常出现排便时剧烈疼痛及鲜红色出血。
- 炎症性肠病(IBD):包括溃疡性结肠炎和克罗恩病,在泰国较少见。症状可包括血性腹泻、腹痛、乏力及体重不明原因下降。
- 缺血性结肠炎:因结肠血流不足导致肠壁缺血坏死,表现为腹痛、压痛及血性腹泻。
- 憩室病:憩室感染或憩室颈部血管破裂时,可引起腹痛及消化道出血。
- 性传播感染(STI):如淋病、衣原体感染、单纯疱疹病毒及梅毒,可引起直肠黏膜炎症导致出血;肛交亦可能造成局部刺激或损伤。
- 结肠炎:可由感染或自身免疫性炎症引起,常伴有发热、腹痛及带血黏液便。
- 血管发育异常(血管扩张症):指肠壁异常或脆弱血管,易在粪便摩擦下破裂出血。
- 消化性溃疡:多由幽门螺杆菌感染或长期使用非甾体抗炎药(如阿司匹林、布洛芬)引起。
- 结直肠息肉或结直肠癌:常引起隐匿性出血,肉眼不易察觉,多在筛查中发现。
- 食管静脉曲张或 Mallory–Weiss 综合征:可导致严重上消化道出血,表现为呕血或黑便。
- 抗凝药物:如阿司匹林或华法林,可能增加胃肠道出血风险,有时会导致黑色大便。
- 细菌性胃肠炎:由大肠杆菌、沙门氏菌、志贺菌或弯曲菌引起,可导致血性腹泻、恶心、呕吐和腹部绞痛。
- 子宫内膜异位症:若累及肛门附近或直肠壁,可在月经期间引起直肠出血。
- 胃肠道出血:可发生在食管、胃、结肠、直肠或肛门,表现为呕血、黑色柏油样大便或新鲜血便。伴随症状可能包括乏力、头晕、胸闷或呼吸困难。

儿童大便带血的常见原因
儿童出现大便带血,可能由多种原因引起,既可能是轻微问题,也可能与较严重的疾病有关。常见原因包括:
- 便秘:便秘是儿童直肠出血最常见的原因。由于大便干硬或排便用力,可能导致肛门黏膜受损,从而出现出血。
- 消化性溃疡:消化性溃疡多与幽门螺杆菌(Helicobacter pylori)感染有关,常见症状包括黑色柏油样大便(黑便)、上腹部疼痛或频繁打嗝。
- 食物过敏:对牛奶蛋白、鸡蛋、花生、小麦、鱼类或海鲜等食物过敏,可能引起肠道炎症和出血。这些过敏原有时来自配方奶,或可通过母乳传递。
- 感染性腹泻:进食或饮用被病毒、细菌或寄生虫污染的食物或水,可导致感染性腹泻,并可能伴随大便带血。
- 美克尔憩室(Meckel 憩室):这是一种先天性小肠末端憩室,部分憩室内含有分泌胃酸的胃黏膜组织,可引起消化道出血。该病多见于幼儿,通常可通过手术切除治疗。
- 炎症性肠病(IBD):包括克罗恩病和溃疡性结肠炎,属于慢性肠道炎症性疾病,也可能导致大便带血。

便血的病因如何诊断?
- 鼻胃管灌洗(Nasogastric lavage)
通过鼻腔插入一根管子进入胃内,抽吸胃内容物,用于判断是否存在上消化道出血。 - 胃镜检查(食管胃十二指肠镜,EGD)
将一根细小、柔软的内镜经口腔进入食管、胃及十二指肠上段,用于查找出血来源。检查过程中如有需要,可取组织进行活检。 - 结肠镜检查(Colonoscopy)
将内镜经肛门进入结肠,观察结肠内部情况,可发现出血点、炎症、息肉或肿瘤,并可取组织样本进行病理检查。 - 胶囊内镜(Enteroscopy)
患者吞服一枚带有摄像头的胶囊,用于拍摄小肠内部影像,适合检查常规胃镜和肠镜无法到达的小肠区域。 - 钡灌肠 X 线检查(Barium X-ray)
通过口服钡剂或灌肠方式,使消化道在 X 线下显影,帮助发现结构异常。 - 放射性核素扫描(Radionuclide scanning)
静脉注射少量放射性示踪剂,利用特殊摄像设备追踪其分布,从而定位出血部位,适用于间歇性或少量出血。 - 血管造影(Angiography)
将造影剂注入血管后进行 X 线成像,若存在活动性出血,可观察到造影剂外渗,从而精确定位出血血管。 - 计算机断层扫描(CT)
可用于发现炎症、肿瘤、憩室病变及其他可能导致消化道出血的原因。 - 剖腹探查术(Laparotomy)
属于开放性腹部手术,仅在其他检查手段无法明确出血原因时,作为最后手段使用。
血便或直腸出血如何治疗?
由便秘引起的直肠出血通常无需特殊治疗即可自行缓解。在轻度情况下,医生可能会建议采用高纤维饮食,以缓解便秘并减少排便时用力,同时配合规律的体育活动,以促进正常的肠道功能。
若症状较为严重,或出血由其他原因引起,治疗方式可能包括:
- 药物治疗:
如使用抗生素治疗幽门螺杆菌(H. pylori)感染;使用抑制胃酸的药物治疗胃溃疡;或为炎症性肠病患者使用抗炎药物。 - 手术治疗:
切除息肉、癌变或受损的肠段,发炎的憩室,或因慢性炎症性肠病而受影响的肠段。 - 内镜止血治疗:
在内镜检查过程中,采用注射治疗、热凝固、激光治疗,或对出血血管进行结扎/夹闭等方式以达到止血目的。 - 血管造影介入治疗:
通过血管造影将药物直接送至出血部位,以协助控制出血。该方法通常在其他治疗方式未能奏效时采用。
大便带血症状概述
直肠出血或大便带血是胃肠道疾病的重要症状之一。其病因范围广泛,从较轻的痔疮、肛裂,到严重的结直肠癌均可能引起。血液的颜色可为初步判断出血部位提供线索:
- 鲜红色血液:常提示下段大肠或肛门病变。
- 暗红色或黑红色血液:可能来自更高位的消化道,如结肠或小肠。
无论何种情况,出现大便带血都应及时就医,明确病因并制定合适的治疗方案。治疗方式可能包括药物、内镜操作或外科手术。
就诊前准备
在就诊前,建议患者记录症状出现的时间、频率及伴随表现,並准备好要咨询医生的问题,例如:
- 我的情况是否严重?
- 您建议进行哪些检查和治疗?
- 我该采取哪些措施缓解症状或预防复发?
常见问答(FAQ)
- 发现大便带血需要担心吗?
需要高度重视。大便带血可能是胃肠疾病的警示信号。若出血频繁、持续超过一周,可能导致贫血,严重时甚至休克,应立即就医。
- 大便带血是否总是严重问题?
不一定。轻度便秘或肛裂也可能导致出血,并可自行缓解。但仍需医生评估,以排除严重疾病。
- 鲜红色血液比黑色血液更危险吗?
鲜红色血液通常来自肛门或直肠;黑色柏油样大便则提示上消化道出血,如胃或小肠。无论颜色如何,都应尽快接受医学评估。
- 排便用力会导致出血吗?
会。过度用力可能引起痔疮或肛裂,这是常见的直肠出血原因。
- 儿童与成人的出血原因是否相同?
不同。儿童常因便秘导致肛裂或感染性肠炎而出血;成人则更常见慢性疾病,如炎症性肠病、憩室病或结直肠癌。
- 男女之间的出血原因有差别吗?
总体相似。但部分女性在月经期间因激素变化或盆腔压力增加,可能出现直肠出血。
- 食物会导致大便呈红色吗?
会。食用甜菜、黑莓、番茄或含红色食用色素的食物后,大便可能呈红色。铁剂或某些药物也可能使大便变黑。
医生提醒
大便带血可能由轻微且可治疗的问题引起,也可能是需要紧急处理的严重疾病。及时就医是获得准确诊断和正确治疗的关键步骤,不仅能提高治愈率,还能有效预防并发症。

















